Interesting Case Of Type A Dissection Of Aorta - Dr. Swati Shah
Salient Points :
- • Resource constraint
- • Multiple repairs
- • Absent Innominate artery
- • Anomalous origin of Rt. Subclavian Artery
- • Narrowing of Internal Carotid
- • Post Covid
Solution had to be tailored :
- • Long pump run
- • Long periods of circulatory arrest
- a. Differential circulatory arrest
- b. Continue Antegrade cerebral and lower limb perfusion
- • Time sequence of steps to minimize perfusion time
Anaesthesia, Surgical & Perfusion Technique :
Intermittent Differential circulatory arrest with unique use of Foley’s catheter for Arch replacement with Valve sparing root replacement and mitral valve repair in Marfan’s with Type A dissection.
Sanjeeth Peter, MCh; Manish Das, MCh; Swati Shah, MD. DDMM Heart Institute, Nadiad
Introduction :
Type A dissection of the aorta extending to the bifurcation in Marfan’s syndrome is known to occur. Treatment decisions are challenging in a resource constrained situation when associated with severe LV dysfunction with an EF of 20%, severe Mitral regurgitation & Aortic regurgitation, absent innominate artery with narrowing of Rt. Internal Carotid artery and anomalous origin of Rt Subclavian artery from descending thoracic aorta in a 4-month post-partum 26 yr old woman, who was found to have Covid-19 at elective screening with a lung involvement on HRCT.
Pre-operative CT Aortogram confirmed that the dissection did not involve any of the three arch vessels (Rt. common carotid, Lt. common carotid & left subclavian artery) or the Rt. subclavian artery whose origin was from the true lumen of the descending thoracic aorta. CT angiogram of the head and neck revealed 80% narrowing of the Rt. Internal Carotid Artery at the bifurcation and intact Circle of Willis.

Carotid Angiogram shows 80% stenosis of right internal carotid artery
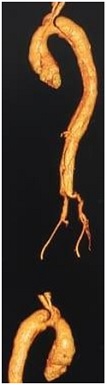
CT Aortogram shows abnormal origin of right subclavian artery from descending thoracic aorta
Mitral & Aorticvalve repair, aortic root replacement, Replacement of Ascending and arch of aorta with frozen elephant trunk as 1st Stage and endograft placement in descending thoracic aorta as a 2ndstagewas planned.
She was kept in isolation under medical supervision and scheduled for surgery 4 weeks after her initial diagnosis when she was confirmed covid negative through recommended tests.
Anaesthesia Technique :
Patient was premedicated with tab. lorazepam 1 mg and tab. pantoprazole 40 mg the night beforeand tab. diazepam 2.5 mg in the morning on the day of surgery. Metoprolol 12.5 mg was given on the day of surgery.
Monitoring included: pulse-oximetry, electrocardiogram, arterial blood pressure monitoring via left radial & left femoral artery, central venous pressure monitoring via the right internal jugular vein, capnography, oesophageal and skin temperature and urine output. 16 Gauze peripheral IV cannula was secured anticipating excessive bleeding. All standard COVID-19 precautions were taken.
General anaesthesia was induced with midazolam (0.05mg/kg), fentanyl (2mcg/kg), thiopental sodium (5mg/kg) and Vecuronium (0.2mg/kg). Trachea was intubated with 7 no. portex endotracheal cuff tube.14 no. Ryle’s tube was inserted post intubation.
Maintenance of anaesthesia was done withtotal intravenous anaesthesia using continuous infusion of Propofol & midazolam/fentanyl/Vecuronium adjusted as per requirement during surgery.
The drugs used for neuroprotection during cardiopulmonary bypass (CPB): methylprednisolone 1 gm, mannitol (20%), 0.5 gm/kg, sodium thiopental 1 gm, furosemide 20 mg.
After weaning off from CPB, the patient was in second degree heart block. Isoprenaline, Dobutamine and Adrenaline infusion were required to maintain hemodynamics. She received 3 units of red blood cells on CPB and 5 units of red blood cells, four units of fresh frozen plasma and four units of platelets were given post CPB after protamine. Methylprednisolone 1 gm was repeated post CPB. Her blood sugar was maintained below 150 mg. She was shifted to the ICU with normal sinus rhythm and stable hemodynamics.
In the ICU, she was stable on 1st post op day. Methylprednisolone 1gm was continued 12 hourly for 24 hours. She was awake 8 hours after surgery with no neurological deficit. Inotropes were gradually tapered and weaning started. Post-operative echocardiography showed improved LV function, LVEF 45%, repaired aortic & mitral valve with normal movement and no pulmonary hypertension. She was extubated 36 hours post-op. Six hours post-extubation, she became tachypneic & disoriented. She was reintubated electively after sedation & put on ventilator again. Post- reintubation chest x ray showed bilateral pleural effusion & haziness. Right sided intercostal drain was inserted and 150 ml fluid was drained. Her airway pressure was remaining high. There was no evidence for septicaemia or any vital organ dysfunction. There was no fever, WBC count was normal, all other blood reports were within normal limit. Respiratory care given was given via nebulization & physiotherapy. She was given dexamethasone 4 mg 12 hourly, piracetam 1.2 gm 12 hourly and citicolin 500 mg 12 hourly as prophylactic neuroprotection for 5 days. She was kept on the ventilator for 3 days and respiratory care continued. She was extubated on post op day 7 with stable hemodynamics and shifted to ward on 10th post-op day. She was discharged on the 12th post-op day.
Surgical steps :
After all the arch vessels were dissected free from surrounding tissue, cardiopulmonary bypass was initiated through right femoral artery and bi-caval cannulation. The ascending aorta was cross-clamped and the heart arrested through retrograde cardioplegia. Cooling was initiated and the mitral valve was repaired using a 28mm ‘Physio’ ring. The aorta was transactedjust above the STJ and the dissection was found to extend into the Non coronary sinus.Separate origin of LAD and LCX was noted. The Sinuses were excised and coronary buttons were prepared for a valve sparing root replacement using Valsalva graft.
With the core temperature having reached 18oC, the arch vessels were clamped individually, a cross clamp applied across the aorta beyond the left subclavian. The aortic arch was opened and the Left carotid artery was cannulatedand antegrade cerebral perfusion initiated @ 100 ml per minute. Femoral perfusion was stopped, descending aortic cross clamp removed and the aorta was transacted beyond the left subclavianartery origin. The layers of dissection were identified and the origin of right subclavian artery about 3 cms beyond the transection was noted. In order to protect distal vital organs, beyond the descending aorta, a foley’s catheter (with 50cc capacity bulb) was passed ante-gradely into the descending aorta and the bulb was inflated up to 40 cc, adjusting the volume of the balloon so as to occlude the flow when femoral circulation was restarted 5 minutes later. The layers of the descending aorta were then sandwiched using strips of felt. An elephant trunk graft was prepared with an opening for the origin of Rt. SCA. Femoral circulation stopped (3 minutes), foley’s catheter removed and re- inserted through the elephant trunk graft. This was then positioned inside the descending aorta aligning the opening for the Rt. SCA.
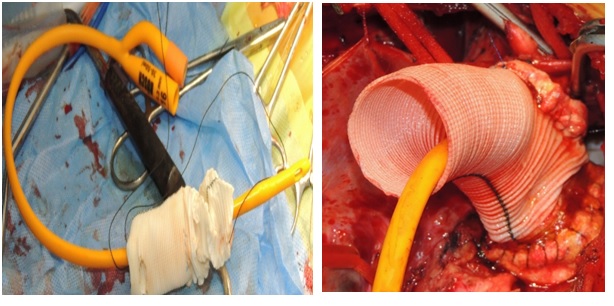
Foley's catheter as a endoclamp
The anastomosis was completed, femoral circulation momentarily stopped, intussuscepted graft pulled out, foley’s reinflated and femoral circulation restored and patient was warmed up to 22oC. An opening for the arch vessel island was made in the graft.The foley’s was now repositioned through the arch opening and anastomosis begun on the posterior margin.
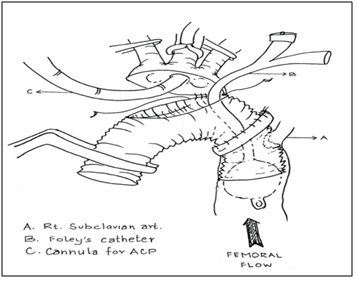
ACP & Distal perfusion
When a few cms of the anterior margin was remaining, circulation was again momentarily stopped, the Carotid catheter and the foleys catheter were removed, arch anastomosis completed and after de-airing, femoral circulation restarted clamping the proximal end of the arch graft and warming to normal temperature initiated. During re-warming, aortic valve repair, root replacement using Valsalva graft was performed and both ends of the grafts were anastomosed. Finally, after warm blood given retrogradely through coronary sinus, the cross clamp was released and the patient was weaned off CP bypass.
- • Total surgical time : 11 hours
- • CPB time : 6 hrs 8 mins.
- • Cooling time : 50 mins.
- • DHCA time : 30 mins, with total 2 mins without cerebral perfusion and 7 mins without distal perfusion.
- • Rewarming time : 2 hrs 35 mins.

Final result
Discussion :
The aim of surgery, anaesthesia and the perfusion technique is to treat the life-threatening aortic pathology and neurological as well as vital organ protection during surgery
It is becoming clear that Covid-19 infection affects multiple systems. The duration and severity of disease, time after recovery and presence of other co-morbidities probably plays a role in the outcomes after surgery. When extensive surgery is planned especially in a patient who hasrecently recovered from Covid-19, duration of CP Bypass and circulatory arrest must be minimized. Absence of an Innominate artery and 80% narrowing of the Rt. Internal Carotid prevented making a ‘Rt Carotid to Rt. Subclavian’ graft lest the narrowing in the Internal Carotid contributes to a ‘steal’ effect. Hence direct cannulation of the left carotid artery, after opening the arch, was done for ACP. Resource constraints prevented the use of hybrid grafts (thoraflex) and Neuromonitoring like Bisprectal Index(BIS) or Cerebral oximetry. In addition, the origin of the Rt SCAhad to arise from the graft. An opening was made in the descending limb of the graft which aligned with the origin of the SCA. The descending limb with the tip marked would serve as a landing for the endograft. A Foley’s catheter with a balloon capacity of 50 cc (but in this case inflated up to 40cc) , was used as an endoclamp to ensure a bloodless field and isolate the lower body arterial system and maintain femoral perfusion. Body temperatures were maintained at 22-24oC, so as to permit use of low flows which prevented dislodgement of the Foley’s. Use of Femoral arterial cannulation, Carotid artery cannulation and Foley’s catheter as Endovascular clamp permitted Intermittent momentary circulatory arrest and Differential circulatory arrest ensuring adequate perfusion throughout the body preventing prolonged duration of Circulatory arrest and CP bypass.
Since the patient had a history of COVID-19, post-operative re-intubation & delayed lung recovery could be due to the COVID induced inflammatory changes in the lungs [9]. Her postoperative recovery was otherwise uneventful.
Deep – moderate hypothermia with antegrade perfusion through left carotid artery, methylprednisolone, thiopental, mannitol and furosemide as an adjuvant for cerebral protection and continuous distal vital organ perfusion offers a relatively uncompromised surgical field, avoids clamp injuries of the vessels minimizing the risk of micro and macro embolic events. This technique also eliminates the “time factor” in aortic arch repair and allows meticulous anastomosis.
References :
- • Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study; Lancet
- • Extrapulmonary complications of COVID‐19: A multisystem disease? Journal of Virology
- • Timing of surgery after recovery from coronavirus disease 2019 (COVID-19) infection ; Infection Control & Hospital Epidemiology (2020), 1–2
- • Totally Normothermic Aortic Arch Replacement Without Circulatory Arrest; ATS 2003
- • Neurologic outcome after ascending aorta-aortic arch operations: effect of brain protection technique in high-risk patients; J Thorac C ardiovasc Surg. 2001; 121:1107–21.
- • A study of brain Comparative protection during total arch replacement comparing antegrade cerebral perfusion versus hypothermic circulatory arrest, with or without retrograde cerebral perfusion: analysis based on the Japan Adult Cardiovascular Surgery Database
- • Total debranching hybrid total arch replacement with a novel frozen elephant trunk for acute aortic dissection type A ; JTCVS
- • The Buffalo Trunk Technique for Aortic Arch Reconstruction; ATS
- • Study finds lung impairment in recovering covid 19 patients/www.cidap.umn.edu> 2020/06
News And Update
© Copyright ACTA Mumbai 2020. All Rights Reserved.

